Frequent, universal COVID-19 testing has been one of the chief preventive methods used in long-term care facilities (LTCs). Although only 8% of COVID-19 cases occur in LTCs, these cases have accounted for 40% of all reported COVID-related deaths. Many facilities have employed the Center for Medicare and Medicaid Services’ (CMS) recommendation to frequently test their employees and residents for COVID-19. However, this is resource-intensive and has met numerous challenges in implementation and logistics at most of them. In addition, many LTCs experienced COVID-19 outbreaks despite following the CMS recommendations on testing.
“In the US, we tend to pay more attention and focus on expensive tests and therapeutics to combat this pandemic. Many of those have limited or marginal benefits,” Michihiko Goto, MD, assistant professor in Infectious Diseases, said. “Still, there are many inexpensive and very effective low-tech interventions we can use” to slow the spread of the virus.
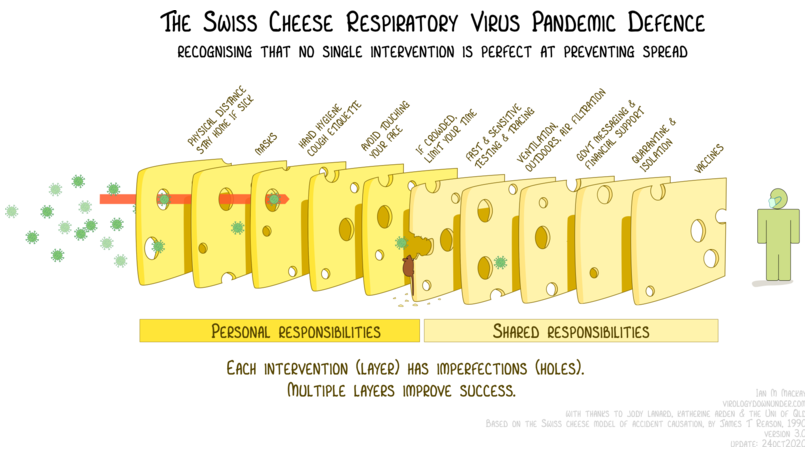
The VA Midwest Health Care Network (VISN-23) took a different approach from routine and widespread testing, relying instead on a variety of measures. These multimodal measures have become commonly referred to as the “Swiss cheese” approach, implying that, despite the limitations inherent within each measure, when combined they prove effective.
In a new publication, Goto and Eli Perencevich, MD, professor in General Internal Medicine and of Epidemiology, detail the successful measures VISN-23 implemented. Thanks to these measures, even without frequent testing, the 20 long-term health care units in nine VA facilities across the five states that comprise VISN-23 were able to maintain zero resident infections of COVID-19 for six months. Their study, currently in preprint, will be published in Infection Control & Hospital Epidemiology.
“Unfortunately, COVID-19 outbreaks still have been reported from community long-term care facilities that implemented frequent testing per CMS recommendations,” Goto said. “Relying on just one measure with visibility is not enough and can potentially make the facility less safe if not used in conjunction with many other measures.”
As soon as the virus was reported in the region on March 6, VISN-23 began its new procedures, requiring new patients to quarantine for 14 days and limiting visitations to those critical for providing care. Each visitor was screened for symptoms and had their temperature measured before entering the facilities. All residents were screened daily for fever and symptoms. The facilities also reduced their staff and educated the remaining staff on proper hand hygiene and respiratory etiquette.
In late March, VISN-23 also implemented a universal face shield mandate. Furthermore, once COVID-19 became more prominent in the region at the beginning of April, face masks were provided and required for all employees. Residents were also required to wear face masks unless they were in their private rooms.
Testing was reserved only for residents who presented with fever or symptoms of COVID-19. In each instance over that six-month period, all residents tested negative. In late April, in response to high levels of community spread and concern over outbreaks at many other LTCs, a universal testing of staff was implemented to reveal that only four employees were positive though asymptomatic. Contact tracing revealed that these cases were community-acquired and not staff-to-staff transmission.
“This success was possible only because we have outstanding frontline care teams at long-term care units in VISN-23 who diligently followed basic infection prevention measures and our recommendations,” Goto said. “Many community long-term care facilities are understaffed and do not have the luxury to have infection control experts readily available, but we have been very fortunate to have on-site infection control professionals and facility leadership that placed priorities on long-term care units at all facilities.”
When the analysis of the VISN-23 measures concluded on Sept. 1, none of the nearly 500 VA Midwest Health Care Network residents had tested positive. The study estimated that 20,000 tests were saved during the six-month period. By limiting testing to those with symptoms and taking proactive prevention measures, resource-stress was limited, in addition to preventing COVID-19 mortality and morbidity for the residents.
“Beyond the specific interventions, this study highlights the importance of strong support from executive leadership teams, infection control professionals, hospital epidemiologists, and all clinical staff on the care units,” Perencevich said.
Goto agreed. “Let us give the largest credit to those frontline staff members, on-site infection control professionals, and leadership teams,” he said.
Goto and Perencevich worked with Nicole Ueckert, RN, and Robert Meiches, MD, on the study.