Previous studies have found that manipulating renal nerves could serve as a hypertension therapeutic in cases where pharmacological treatment is ineffective. Sailesh Harwani, MD, PhD, assistant professor in Cardiovascular Medicine, has conducted the first study that suggests the integration of adrenegic, cholingeric, and renal systems affects the development of premature hypertension. His study also is the first to demonstrate that the expression of certain renal sodium transporters appears to be, at least partially, regulated by the presence of a specific inflammatory immune cell population in the kidney.
The study, involving multiple members of the Abboud Cardiovascular Research Center, was published in the American Physiological Society’s American Journal of Physiology – Heart & Circulatory Research (AJP-Heart). Harwani was invited to discuss his study on a podcast with the program’s editor-in-chief Irving Zucker, PhD, of the University of Nebraska Medical Center and Liang Xiao, PhD, of Vanderbilt University.
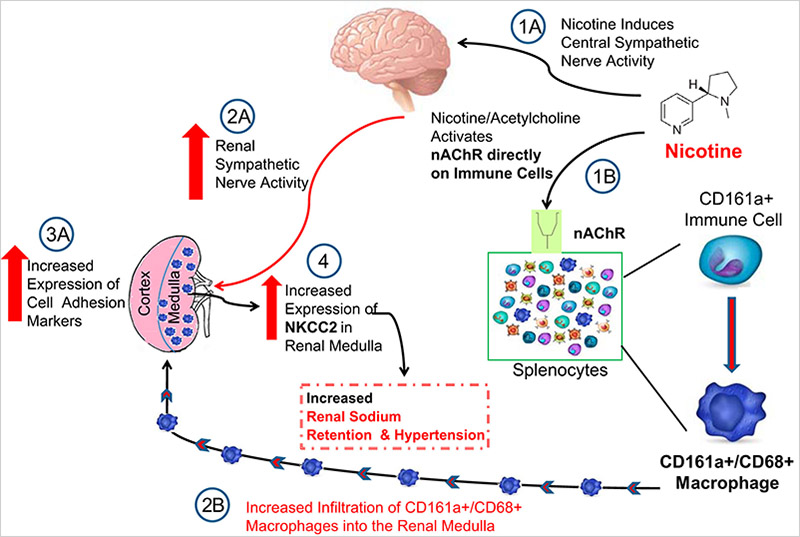
Using a genetic model for essential hypertension, Harwani investigated the coordinated role of the adrenergic and cholinergic nervous system in mediating renal inflammation. Harwani’s study shows that activation of cholingeric receptors on immune cells leads to expansion and differentiation of inflammatory macrophages and that renal adrenergic nerves influence the migration of inflammatory immune cells/macrophages into the inner portion of the kidney, i.e., the renal medulla.
“Thus, we are showing how the two arms of the nervous system coordinate to lead to inflammation of the kidneys and the development of hypertension,” Harwani said. “The study utilizes immune-based therapy to remove the inflammatory cells from the circulation and shows that there is promise for such immune-based therapies for the treatment of hypertension and kidney disease.”
Harwani’s study included collaborations with fellow University of Iowa researchers François Abboud, MD, professor in Cardiovascular Medicine; David Meyerholz, DVM, PhD, professor of Pathology; Peter Snyder, MD, professor in Cardiovascular Medicine; Nandita Raikwar, PhD, assistant research scientist in Harwani’s lab, and former undergraduate researcher Cameron Braverman. Robert Fenton, PhD, professor of Biomedicine at Aarhus University in Denmark, also contributed to the publication.
Continue the conversation! Follow Sal Harwani on Twitter @docharwani, the American Journal of Physiology-Heart & Circulatory Physiology @AJP-HeartCirc, or Internal Medicine @IntMedatIowa.